October 18 through 24, 2021 was National Addiction Treatment Week. The goal of this week is to highlight the critical treatment gap between the number of patients who need addiction treatment and qualified medical professionals available to treat patients using evidence-based approaches.
Over the course of the week, we shared addiction statistics along with action steps on our social channels. Our goal is to amplify the message of this initiative, encourage further discourse among professionals, and raise awareness for individuals struggling with addiction so that they can feel safe and supported getting the help they need. Together, we can disrupt the cycle and challenge inequities in the system so that everyone can recover.
Please feel free to share this post and the associated links on social media and beyond to spread the message and resources.
Risk Factors for Addiction
Risk factors for addiction can be divided into three categories: biology, environment, and development. (Source: National Institute on Drug Abuse)
Research-based programs preventing the early use of drugs or alcohol may go a long way in reducing these risks. That being said, we think that more people need access to programs that promote mental wellness, offer a network of support, and make recovery an option for everyone.
It’s important to remember that addiction is a disease that can affect ANYONE, and that substance use can change the brain. When a mental health crisis escalates without support, the consequences can be devastating. Those who witness a mental health crisis may not feel equipped to offer support, so they might reach out to law enforcement with good intentions. Unfortunately, this can further escalate the situation.
The Crisis Assistance Helping Out on The Streets (CAHOOTS) program in Eugene, Oregon provides a model for dispatching mobile teams of health care and crisis workers, rather than law enforcement, to respond to individuals experiencing a mental health or substance use disorder crisis.
You can take action and cosponsor the CAHOOTS Act which would provide funding to help states adopt mobile crisis response models, based on the CAHOOTS program. Add your name to the act, share the opportunity, and amplify the effort to support more people struggling with addiction.
Co-Occurring Disorders
More often than you might imagine, drug or alcohol addiction can mask mental illness, or vice-versa. It’s estimated that as many as half of those with substance addictions also suffer from mental health disorders. Conversely, at least a quarter of those with mental illness also suffer from addiction.
One way we can disrupt the cycle of addiction is by supporting organizations that develop and expand services for individuals with substance use disorders and co-occurring disorders.
The Mental Health Justice Act would provide funding and technical assistance for mental health provider first responder units. These units could respond to mental health and substance use crises, diverting dependence on police in the event of a crisis. As a result, individuals struggling with addiction and mental health issues would be less likely to end up in jail after incurring charges for minor nonviolent offenses. Instead of waiting to receive care in an already overwhelmed criminal system, someone in crisis could receive the support and care that they need immediately.
You can cosponsor the Mental Health Justice Act by adding your name to the petition.
The Role of Prescription Drugs in the Opioid Epidemic
Addiction is on the rise, and prescription drugs are the leading cause. More than 15 million Americans suffer from prescription drug addiction at any given time. Research suggests that doctors are prescribing potentially addictive drugs at needlessly high rates.
Along with overprescribing highly addictive drugs, most health care providers are not equipped to identify, treat, and help patients manage addiction. As a result, many people struggling with addiction are unable to get the support they need in order to pursue recovery. The good news? Opioid dependence is preventable, but first, we need more education around safe medication management.
We believe that all health care providers should be required to have a working understanding of addiction before they are allowed to prescribe addictive narcotics. If more health care providers were educated about the risks associated with opioid prescriptions, they would be more likely to pursue other pain management options for their patients and provide more education around highly addictive substances.
You can take action to support the Medication Access and Training Expansion (MATE) Act, a bill that would require prescribers to undergo opioid and substance use disorder training before receiving or renewing their license to prescribe controlled substances.
Alcohol Addiction
An estimated 95,000 people (approximately 68,000 men and 27,000 women) die from alcohol-related causes annually, making alcohol the third-leading preventable cause of death in the United States. (Source: CDC)
The CDC is working to make alcohol screening and brief intervention (SBI) a routine part of health care in primary care settings. Alcohol SBI is a preventive service that can occur as part of a patient’s wellness visit. This service will help to identify individuals who are drinking more than the recommended amounts and offer referrals when appropriate. Health care providers can incorporate alcohol screening into their practice ahead of the CDC efforts.
To raise awareness for alcohol addiction, we’re sharing the CDC guidance for alcohol SBI along with the CAGE questionnaire for alcohol use. This questionnaire consists of 4 simple and easy-to-remember questions used to screen for alcohol dependency. The CAGE acronym stands for Cut, Annoyed, Guilty, and Eye-opener, keywords that help you remember each question from the list below:
- Have you ever felt you should cut down on your drinking?
- Have people annoyed you by criticizing your drinking?
- Have you ever felt bad or guilty about your drinking?
- Have you ever had a drink first thing in the morning to steady your nerves or get over a hangover?
These questions can help us reflect on our relationship with alcohol and see if dependency on alcohol may be a concern.
Access to Treatment
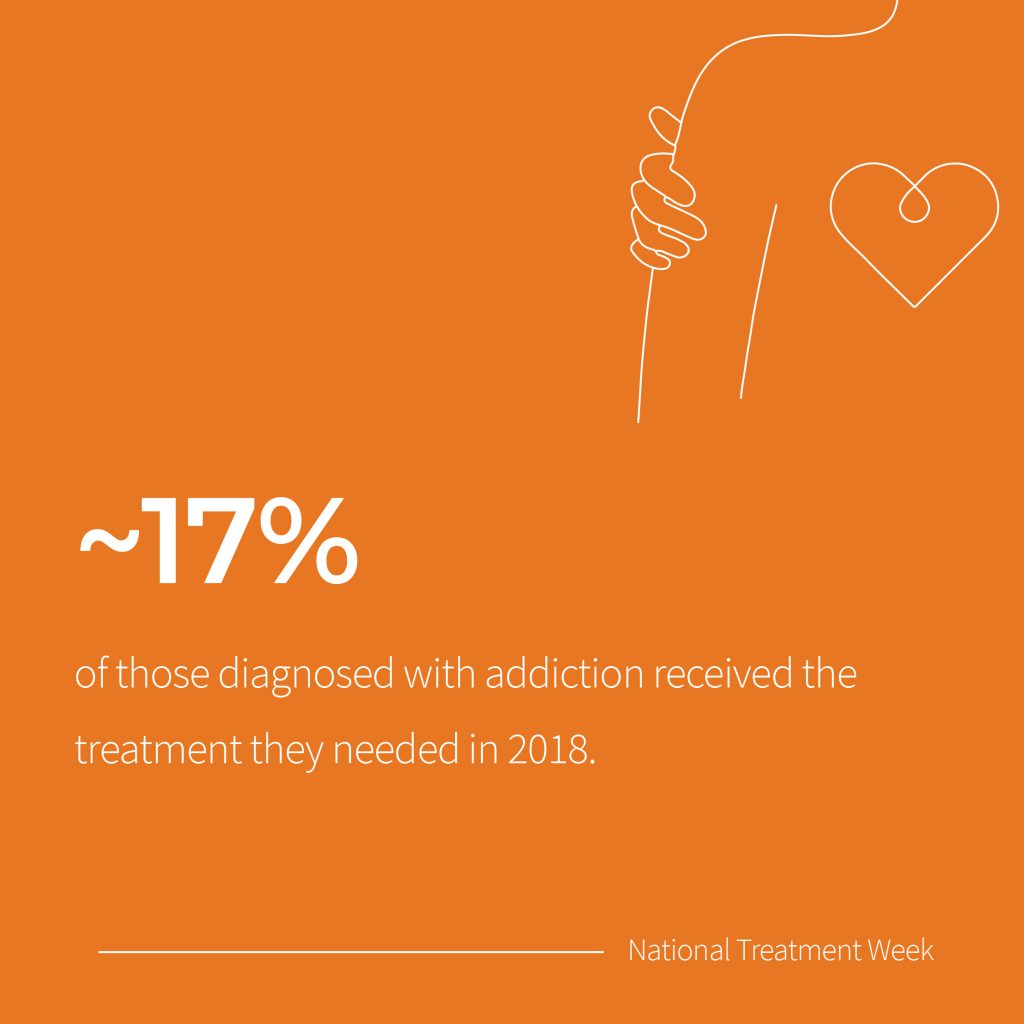
In 2018, an estimated 2 million Americans were addicted to opioids, yet only about 400,000 people received treatment at a specialty facility. (Source: SAMHSA)
In that same year, an estimated 14.8 million adults had alcohol use disorder, yet only 686,000 (5%) received treatment as a specialized facility. (Source: SAMHSA)
According to the Partnership To End Addiction, “The Mental Health Parity and Addiction Equity Act (Parity Act) requires most health plans to cover mental health and substance use disorder treatment the same way they cover treatment for any other disease. Despite strong legal protections, millions of families still struggle to get insurance coverage for needed treatment and are unaware of their rights to affordable care due to weak enforcement and poor implementation of the law.”
With your support, we can urge lawmakers to increase insurance coverage and access to affordable care. You can learn more about The Mental Health Parity and Addiction Equity Act and take action by emailing your members of Congress and asking them to cosponsor the Parity Enforcement Act (H.R. 1364).
Looking Ahead
During National Addiction Treatment Week, we’ve highlighted statistics and resources to help raise awareness around the critical treatment gap between the number of patients who need addiction treatment and qualified medical professionals available to treat patients using evidence-based approaches. We’ve shared action steps from the Partnership To End Addiction so that you can help make real changes and increase resources for individuals struggling with addiction.
This year, National Addiction Treatment Week is layered with a bit more urgency: with the pandemic, the treatment gap will be even wider.
Addiction in the Midst of the Pandemic
“Anxiety and depression are up three to four times what they were pre-pandemic,” says Dr. Jerry Vaccaro, President of All Points North Lodge. “Substance use disorders have at least doubled. The CDC reports that more than 87,000 Americans died from an overdose from Sept. 2019 to Sept. 2020, a 20% increase from the previous year. Alcohol consumption is up. Eating disorders have climbed more than 60%. Suicidal thinking is on the rise — anywhere from two to four times, depending on the study.”
“Less than 20% of those who could benefit from addiction treatment actually received it before the pandemic.” Dr. Vaccaro continues, “There isn’t a simple fix to this complex problem. But the need is urgent, and we must respond. Our nation’s well-being and ability to emerge from this pandemic with health in hand are at stake. So where do we begin?”
Education and advocacy are an important first step, and we encourage you to continue to share statistics, resources, and petitions from this post. But we need to prepare for the additional increase in demand for substance use treatment and mental health support that we’re already seeing as a result of the pandemic.
Dr. Vaccaro offers solutions, possible barriers to care, and what to anticipate in a new piece published on Medium’s largest mental health publication, Invisible Illness. Find the full piece from Dr. Vaccaro: “The Pandemic’s Next Wave: Behavioral Health Problems.”
At All Points North Lodge, we’re here to help both via virtual therapy and in-person as you navigate mental health, trauma, and addiction. Contact one of our caring representatives by phone at 855-510-4585 or via to get started. This pandemic is challenging and isolating. Please don’t suffer in silence — we’re here for you.